Unlocking Relief: The Fascinating Connection Between Fascial Health and Ehlers-Danlos Syndrome
Ehlers-Danlos Syndrome (EDS) can bring a variety of challenges to those who experience it, including joint hypermobility, skin fragility, and chronic pain. In your search for effective ways to manage EDS symptoms, exploring the link between fascial health and symptom relief can offer new insights. This blog dives into the fascinating connection between fascial health and EDS, offering guidance on how optimising fascia mobility may alleviate some of the discomfort associated with this condition.
Understanding Fascia Mobility and EDS Symptoms: Fascia, the intricate network of connective tissue throughout your body, plays a crucial role in your musculoskeletal health. Recent research highlights its significance in proprioception – your body's awareness of movement and position. The relationship between fascial mobility and myo-fascial pain, often experienced by those with EDS, sheds light on the potential for managing symptoms more effectively.
Connecting the Dots -> Fascia, Pain, and EDS: Fasciae contain small-diameter fibres that transmit nociceptive (pain) signals, especially in the presence of inflammation. This finding holds particular importance for those with EDS, as pain is a common experience. Myo-fascial pain syndrome, characterised by tender nodules known as "trigger points," is a key aspect of EDS-related discomfort.
Connective Tissue
How To Improve Fascial Health in EDS & Connective Tissue Disorders
The main complication in hyper-mobility is the inability to get healthy muscle contraction. But what is healthy muscle contraction and why is it extremely important?
The following is a MUST read if you suffer from hypermobility and want to gain stability, strength and evenly distrubted tension.
Healthy Muscle Contraction: Muscle contraction begins with a signal from the nervous system, which triggers the release of calcium ions within muscle cells. These calcium ions interact with proteins, primarily actin and myosin, leading to a series of events that result in the shortening of muscle fibers. This process generates force, allowing the muscle to contract and exert movement.
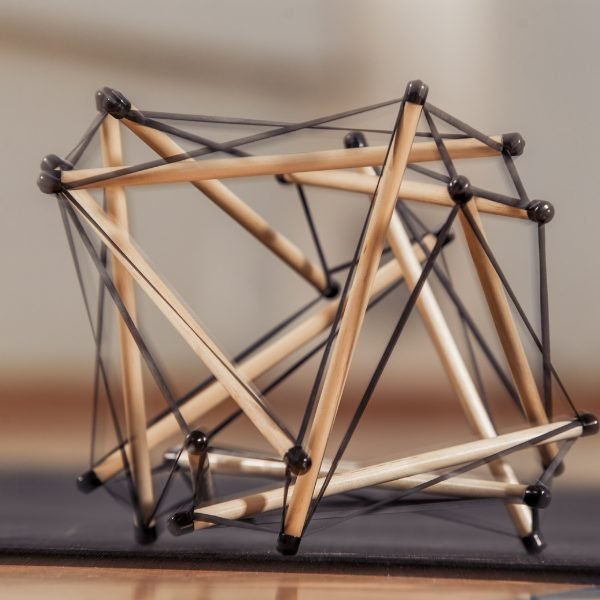
Tensegrity and Muscle Contraction: Tensegrity is a structural concept that describes how tensional and compressional elements work together to create stable structures. In the context of the human body, muscles, bones, and connective tissues form a tensegrity system. Muscles provide tension, while bones and other tissues provide compression. This interconnectedness allows for efficient and balanced movement and stability.
In a tensegrity system, proper muscle contraction is crucial not only for movement but also for maintaining the integrity of the structure. When muscles contract, they generate tension that is transmitted through fascia and other connective tissues to the bones. This tension allows for proper alignment and support, ensuring that forces are distributed evenly across the structure.
Tensegrity Structure: A structure that is held together by evenly distributed tension.
Hypermobility and Muscle Contraction: Hypermobility refers to increased joint flexibility beyond the normal range of motion. While it might seem advantageous, it can actually disrupt the balance within the tensegrity system. Imagine that the above image had some or all of its elastic string components stretched to the point that they were loose. This would cause the structure to lose shape. In hypermobile individuals, the excessive joint movement can lead to laxity in ligaments and connective tissues. This laxity can affect the stability and support provided by muscles.
When muscles contract in hypermobile individuals, the excessive joint mobility can prevent them from generating optimal tension. The lack of proper tension transmission through lax connective tissues can result in decreased stability and compromised movement control. In addition, hypermobile joints are more susceptible to injury due to reduced support from surrounding tissues.
Due to the lack of contractile support, hypermobile individuals also expend more energy to perform simple tasks that require stability. This increased energy expenditure can lead to fatigue and even exhaustion, contributing to the overall feeling of discomfort.
How Hypermobilty can lead To Dehydration & Pain
Dehydration and Fascial Health: Connective tissues, including fascia, play a crucial role in maintaining hydration within the body. Fascia has an intricate network of fluid-filled spaces that help nourish cells and maintain tissue health. In hypermobile individuals, compromised fascial health can impact fluid distribution. Lax fascia may not effectively hold and distribute fluids, leading to a potential for dehydration or inefficient fluid balance within the tissues. Proper hydration is essential for tissue health, and any disruption in fluid dynamics can contribute to discomfort and pain.
Tissue Inflammation and Pain Sensitivity: Lax connective tissues can be more susceptible to inflammation and irritation. When tissues are not properly supported, they can become inflamed more easily, leading to increased pain sensitivity. Inflammation in hypermobile tissues can exacerbate discomfort and contribute to chronic pain conditions.
What Can You Do To Support Your Fascia?
Unlocking Relief through Fascia Mobility: Improving fascia mobility offers promising benefits for managing EDS symptoms:
Enhancing Joint Stability: The key to joint stability is going to be learning to create a healthy muscle contraction and to begin bringing the bodies tensegrity structure back into balance. This is going to include breaking up fascial adhesions while ensuring not to stretch already hypermobile tissue. Rather, focusing on contracting the tissue according to the gait cycle yields the best results.
Tackling Pain: By addressing fascial imbalances and restrictions, you may experience relief from myofascial pain. Techniques such as manual therapy and movement-based therapies (as listed in the point above) can be beneficial. The fasted pain relief comes from identifying and breaking through fascial adhesions and the most permanent relief will come from holding tension and hydration in your tissue through balancing out your gait cycle and improving muscle contraction/elastic potential.
Improving Proprioception: Fascia plays a role in proprioception, impacting how you perceive movement. Optimising fascia mobility can enhance body awareness and movement control. Functional Patterns is proprioception based training as it puts the body in situations in which the correct muscles need to respond to correct stimuli. Some exercises can be detrimental to proprioception as they are unnatural movements (for example, too isolated) for the human body and may not take into account your hypermobility in relation to tensegrity.
Boosting Muscle Function: Addressing fascial restrictions supports better muscle function, which in turn provides additional support to weakened connective tissues. It is a positive feedback loop once you learn to contract your muscles correctly and reduce fascial adhesions.
Personalised Strategies for EDS Relief: EDS symptom management isn't a one-size-fits-all approach. Tailored strategies that focus on optimising fascial health can provide personalised relief:
Biomechanics Training: Targeted exercises that improve movement patterns, joint stability, and muscle engagement can contribute to overall symptom management.
Gait Training: Analysing and enhancing walking patterns can reduce strain on hypermobile joints and improve mobility and pain control. This works in many ways, primarily by evenly distributing tension and improving loading during movement.
Soft Tissue Mobilisation & Myo Fascial Release: Manual techniques that release fascial adhesions and improve tissue flexibility can ease myofascial pain and enhance function.
Enhancing Proprioception: Incorporating exercises to enhance proprioceptive awareness supports better stability and control.
As someone seeking relief from Ehlers-Danlos Syndrome, the connection between fascial health and symptom management is worth exploring. The intricate relationship between fascia mobility and EDS symptoms is an evolving field of study. By understanding the impact of fascia on your condition and symptoms, you can work with healthcare professionals to explore innovative approaches to relief. As research continues to uncover the connection between fascial health and EDS, a more comprehensive approach to symptom management may come to light, offering hope and improved well-being.